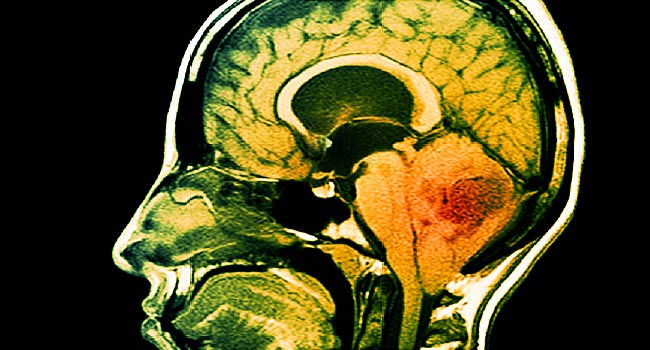
Controlling Brain Cancer Growth By Neuroligin-3 Inhibition : Stanford Research
High-grade gliomas, a group of aggressive brain tumors, cease growing in mice if a signaling molecule called neuroligin-3 is absent or its activity is blocked with drugs, a Stanford team has shown.
High-grade gliomas, a group of aggressive brain tumors, cease growing in mice if a signaling molecule called neuroligin-3 is absent or its activity is blocked with drugs, a Stanford team has shown.
By: Erin Digitale | Stanford News
The growth of certain aggressive brain tumors can be halted by cutting off their access to a signaling molecule produced by the brain’s nerve cells, according to a new study by researchers at the Stanford University School of Medicine.
When the signaling molecule neuroligin-3 was absent, or when its signal was interrupted with medication, human cancers called high-grade gliomas could not spread in the brains of mice, the researchers found.
The study was published online Sept. 20 in Nature. Graduate student Humsa Venkatesh is the study’s lead author.
“We thought that when we put glioma cells into a mouse brain that was neuroligin-3 deficient, that might decrease tumor growth to some measurable extent. What we found was really startling to us: For several months, these brain tumors simply didn’t grow,” said Michelle Monje, MD, PhD, assistant professor of neurology and senior author of the study. The findings suggest that interrupting the neuroligin-3 signal could be a helpful strategy for controlling high-grade gliomas in human patients, Monje added.
High-grade gliomas are a group of deadly brain tumors that include adult glioblastoma, the brain cancer now affecting U.S. Sen. John McCain of Arizona; anaplastic oligodendroglioma; pediatric glioblastoma; and a pediatric tumor called diffuse intrinsic pontine glioma. Five-year survival rates are 60 percent for anaplastic oligodendroglioma, around 10 percent for adult and pediatric glioblastomas and virtually nonexistent for DIPG. New treatments are urgently needed.
Hijacking the normal machinery
The new findings build on prior research published by Monje’s team in 2015. At that time, the scientists showed that neuroligin-3 fueled the growth of high-grade gliomas. This was surprising because the protein is a part of the normal machinery of neuroplasticity in a healthy brain, and it is a relatively new concept that cancer can hijack an organ’s healthy function to drive cancer growth.
In the new study, Monje’s team examined mice that were genetically engineered to lack neuroligin-3. These mice have nearly normal brain function. However, when their brains were implanted with any of the forms of human high-grade glioma, the cancer cells could not proliferate. The growth stagnation persisted for several months.
“Lack of neuroligin-3 doesn’t kill the cancer cells; the cells that are there remain there, but they do not grow,” Monje said. However, 4½ months after implantation, tumors in some mice circumvented their dependency on neuroligin-3 and began to grow again, she added.
Effect specific to high-grade gliomas
The researchers also tried implanting the brains of mice lacking neuroligin-3 with human breast cancer cells. Lack of neuroligin-3 did not affect breast cancer growth, showing that the effect is specific to high-grade gliomas.
The growth-stagnation effects, conserved across different classes of high-grade glioma, were unexpectedly strong. To find out why, the researchers conducted follow-up experiments that examined the cell signals involved in neuroligin-3’s role in the division of glioma cells, which demonstrated that neuroligin-3 activates multiple cancer-promoting signaling pathways and also increases the expression of genes involved in cell proliferation, promotion of malignancy, function of potassium channels and synapse function. The researchers now believe that neuroligin-3 is more than just a gatekeeper of glioma cell division, though further research is needed to clarify its exact role, Monje said.
The team also explored whether blocking neuroligin-3 has therapeutic potential for treating gliomas. Using mice with normal neuroligin-3 brain signaling and human high-grade gliomas, the researchers tested whether two inhibitors of neuroligin-3 secretion could stop the cancers’ growth. One of the inhibitors has never been tested in humans, but the other has already reached phase-2 clinical trials as a potential chemotherapy for other forms of cancer outside the brain.
Both inhibitors significantly reduced glioma growth during a short-term trial, suggesting that the strategy of inhibiting neuroligin-3 secretion may help human patients.
‘Clear path forward for therapy’
“We have a really clear path forward for therapy; we are in the process of working with the company that owns the clinically characterized compound in an effort to bring it to a clinical trial for brain tumor patients,” Monje said. Inhibition of neuroligin-3 will not represent a cure for high-grade gliomas, she cautioned, since it does not kill the cancer cells. Ultimately, she hopes to combine it with other treatment strategies against the tumors.
“We will have to attack these tumors from many different angles to cure them,” Monje said. But given how devastating the tumors are, the possibility of using neuroligin-3 inhibition to slow tumor progression is a hopeful development, she added. “Any measurable extension of life and improvement of quality of life is a real win for these patients.”
The team’s work is an example of Stanford Medicine’s focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.
Other Stanford co-authors are undergraduate Lydia Tam; life science research associate Pamelyn Woo; and graduate students James Lennon, Surya Nagaraja and Shawn Gillespie. Monje is a member of Stanford’s Child Health Research Institute, the Stanford Institute for Regenerative Medicine and Stem Cell Biology, Bio-X, the Stanford Cancer Institute and the Stanford Neurosciences Institute.
Scientists from Dana Farber Cancer Institute, Harvard Medical School and the National Center for Advancing Translational Sciences also contributed to the study.
The research was funded by the V Foundation; the Liwei Wang Research Fund; the National Institutes of Health (grants R01NS092597, 1F31CA200273, P50CA168504 and R35CA210057); the Department of Defense; the McKenna Claire Foundation; Alex’s Lemonade Stand Foundation; The Cure Starts Now Foundation; the DIPG Collaborative; the Lyla Nsouli Foundation; Unravel Pediatric Cancer; the California Institute for Regenerative Medicine; the Childhood Brain Tumor Foundation; the Matthew Larson Foundation; the Joey Fabus Childhood Cancer Foundation; the Wayland Villars DIPG Foundation; the Connor Johnson, Zoey Ganesh and Declan Gloster memorial funds; the N8 Foundation; the Virginia and D.K. Ludwig Fund for Cancer Research; the Stanford Child Health Research Institute; the Breast Cancer Research Foundation; the National Center for Advancing Translational Sciences; and the National Cancer Institute.
Stanford’s Department of Neurology and Neurological Sciences also supported the work.







Leave a Reply